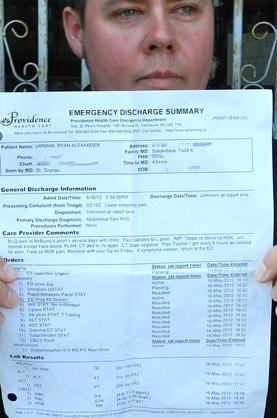
When trans man Ryan Jarman visited the emergency room of St Paul’s Hospital on May 16, he was seeking help for a severe stomach ache that had tormented him for 24 hours. Instead, he received what Jarman describes in his complaint letter to the hospital as medical treatment that left him feeling “violated and traumatized.”
Rather than focusing on the ailment, Jarman alleges that Dr Brian Grunau, the doctor on duty that night, repeatedly inquired about his sexual history after he learned that Jarman is transsexual.
“I answered three or four times that I haven’t been sexually active for a while, and I told him, ‘I had a hysterectomy, and I don’t have any reproductive organs. There is nothing going on down there, I promise you that.’”
Despite this information, Dr Grunau removed Jarman’s underwear and started to examine his genitals rather than his stomach, according to Jarman.
“All I could choke out was, ‘What are you doing?’ and he said, ‘Looking for infections.’”
“You are not supposed to remove a patient’s clothing. At that moment I felt so powerless,” Jarman says.
As Jarman later learned from his blood-work form, Dr Grunau also ran a pregnancy test without his patient’s consent and despite the fact that Jarman had a hysterectomy in 2008, making pregnancy nearly impossible.
Jarman’s story is just one of many, believes Marria Townsend, a physician at Three Bridges Community Health Centre, who hears many stories from her trans patients about their negative experiences with healthcare providers. “I know a lot of people who avoid medical care because they don’t feel safe, and that can have devastating consequences,” she says.
“I can’t comment upon any specific interactions between a doctor and a patient,” says Shaf Hussain, spokesperson for St Paul’s Hospital, “but a follow-up needs to be done with this specific interaction.”
“People are looking at this issue and they are looking at what needs to be done,” Hussain says.
Townsend blames a lack of mandatory sensitivity training and a healthcare system that leaves it to the individual care facility to adopt best practices guidelines for transgender patient care.
“This needs to change at the level of medical education. All the different medical programs need to include in their curriculum specific training on transgender health,” Townsend says.
Like most health facilities in the Lower Mainland, St Paul’s Hospital has no mandatory training program for transgender health, although Hussain points out that voluntary workshops and other events on trans health are occasionally offered.
Jarman would like Dr Grunau to get some sensitivity training, preferably from a doctor already trained in trans health.
When Xtra called Dr Grunau for comment, he hung up and did not respond to requests for an interview. But the hospital’s patient relations department informed Jarman that Dr Grunau feels “deeply sorry” and will write a letter of apology.
“He can’t take it back, but it will be interesting to see what the letter says,” Jarman says. “I hope he really owns up to his behaviour. That would make a difference for me.”
A 2010 report by the US National Center for Transgender Equality shows trans people are more likely to experience discrimination or poor counsel when entering the healthcare system.
According to the report, 19 percent of respondents reported being refused care, while 28 percent said they were subject to harassment and violence. Half of the survey’s participants said they had to teach their medical provider about transgender care in order to receive proper treatment.
“If a person is in a vulnerable position seeking medical care, they shouldn’t have to educate their providers about how to provide care for them,” Townsend says. “Really, that is not right.”
 Why you can trust Xtra
Why you can trust Xtra


