Last fall, Dan wanted to get on PrEP in time for Pride in Palm Springs.
A young gay man from Vancouver, whose name Daily Xtra shortened to protect his identity, he had heard all about the pre-exposure prophylaxis drug from previous trips to the United States.
He knew it was effective and relatively safe. He figured a month would be enough to talk to his doctor, get insurance coverage, and pick up the pills. By the time he was partying in California, he thought, he would have a drug flowing through his veins that has been shown to prevent HIV infection as effectively as condoms.
It was not to be.
It took two rejections and over two months of wrangling with his insurance company before Dan was finally covered. In the end, the experience left him so frustrated he has never filled his prescription, choosing to simply buy unprescribed Truvada through an acquaintance.
In British Columbia, Dan’s experience is sadly typical. While many insurance companies will theoretically cover Truvada in some cases, gay men face repeated rejections, confusion, contradictory directions and misinformation before finally getting covered, if they are at all. Since Truvada costs about $900 a month, insurance is usually the only option.
When Dan first approached his insurer, Pacific Blue Cross, about the medication, they told him they could not cover it because it was supposed to be covered by the province; he would have to get a letter from his doctor saying it was for a different purpose, and fill out an application for a special exception.
Even so, his insurer denied his coverage, saying they did not cover “preventative medication.”
Suspicious of this explanation, Dan asked a coworker if her birth control pills — a preventative measure — were covered by insurance. They were.
Dan complained to his human resources department, and Pacific Blue Cross relented, sending him yet another exception form. Weeks more went by, and finally he was covered. By this time, he had already found another source to discreetly buy Truvada. He says he nearly gave up on the process altogether, but the insurer’s denial irritated him enough to press on.
The barriers to men trying to get insured for Truvada come from all directions at once.
Health Canada has still not approved the drug for HIV prevention, only for HIV treatment, meaning doctors have to prescribe it “off label” for a purpose it’s not officially intended.
If men are lucky and persistent enough to get a prescription, they then have to navigate a maze of insurance bureaucracy, possibly outing themselves to their HR department or boss in the process.
Ironically, it is particularly difficult to get Truvada for HIV prevention in British Columbia because the province gives out the drug for free to people already infected. Insurance companies often deny the drug because they say it is already covered, and then force customers to prove the province has denied coverage.
Bill Coleman, a Vancouver counsellor who specializes in gay men’s health, says it took him three months to get coverage through Manulife Financial. First he had to convince his doctor, who was reluctant to prescribe the drug.
“Basically you have to portray yourself as an irresponsible slut who likes to have lots of unprotected anal sex,” he says.
After that, the process seemed easy. Coleman picked up a month supply of Truvada, and started taking it. He went in for a refill a few weeks later, but was told he had to wait until only a few days before he ran out. When he returned later, he was told the insurance company would no longer cover the drug without a letter from the Ministry of Health saying the province wouldn’t pay for it. After hours on the phone asking to talk to a supervisor, he finally convinced Manulife to cover him for another month while he got the letter.
After extracting a letter from the ministry, Coleman was once again covered, until he went in for his next refill. This time, Manulife told him he needed to turn in yet another form, this time from his doctor. When he sent in the form, the company told him his insurance had once again been denied, and he once again had to convince them it was a legitimate claim.
Coleman estimates he spent 40 hours on the phone with Manulife before his Truvada was covered for good. That’s fine for him, a health professional with extensive knowledge of the system, he says, but what about people without the resources to spend hours on the phone arguing with an insurance company?
“I was only lucky enough to know it wasn’t denied because I knew other people who had been covered,” he says. “And I was assertive enough to push it.”
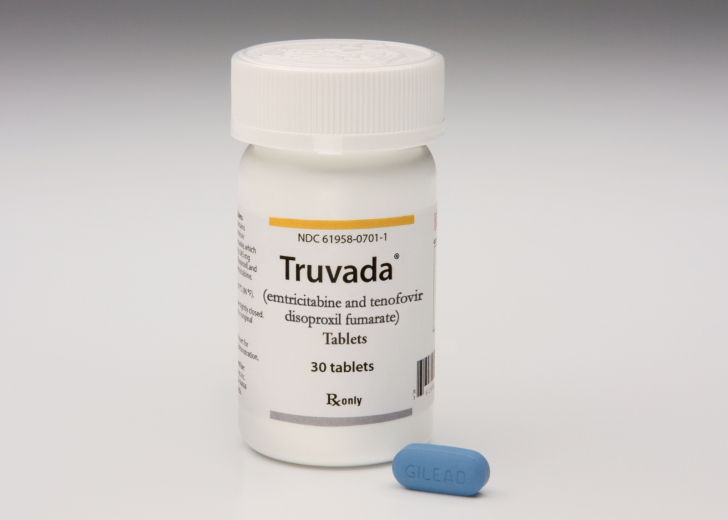
(If gay men are lucky and persistent enough to get a prescription for Truvada in BC, they then have to navigate a maze of insurance bureaucracy, possibly outing themselves to their employer in the process./Gilead Sciences)
When Daily Xtra contacted insurers about the problem, they universally said the responsibility was on employers to make sure their health plan covers Truvada. Joan Weir, a representative of the Canadian Life and Health Insurance Association, insisted that the system works, and the confusion was not intentional obstruction by the insurers.
“I think that’s probably how an employee would see it, but I guarantee that’s not what’s happening at the front line,” she says. “What’s happening is that drugs are coming to committees of medical specialists, and probably some of the frontline staff don’t have all that information.”
“My advice would be to get to the right person at the insurance company to get the right answer.”
As Daily Xtra’s investigation shows, however, that’s not always easy.
When Xtra contacted Manulife’s media relations department, specifically asking about off-label Truvada for HIV prevention, a representative replied that Truvada was covered by the province in BC — perpetuating the same confusion Coleman encountered.
Dean Dawson, a 35-year-old man from Vancouver, was foiled by Manulife, the same company by which Coleman was eventually approved. With the help of his doctor, Dawson did everything right. He was tested, collected all the documentation he needed from his doctor and the province, and sent it in. Manulife denied his application, this time saying the company did not cover “experimental” treatments.
Dawson specifically asked if the problem was his employer or health plan, and the company told him it was not — that Manulife just could not cover the drug at all. Until Health Canada approves the drug for prevention, they said, there was nothing they could do.
“It seems very inconsistent,” Dawson says. “I don’t know if it’s the officer you get or what, but it seems weird that some people can access it and others can’t.”
When Daily Xtra contacted Manulife to explain the discrepancy, a representative wrote that she could not speak to Dawson’s case, but said: “Appeals are reviewed on an individual basis and are assessed according to the information provided and the specific contractual provisions of your group insurance policy.” She did not say if Manulife has a company-wide policy against “experimental” treatments.
Dawson says he will wait, in hopes the federal government moves quickly on Truvada.
In the meantime, he realizes the bitter irony that there is one thing he could do to instantly get as much free Truvada as he wants: contract HIV.


 Why you can trust Xtra
Why you can trust Xtra