The US Food and Drug Administration (FDA) has approved a drug that could significantly reduce the risk of HIV infection in uninfected individuals.
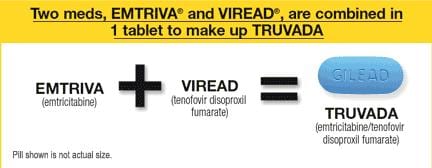
Truvada, a pre-exposure prophylaxis (PrEP) taken daily to prevent infection, was approved for use in conjunction with other safer-sex tools such as condom use and regular HIV testing.
The FDA’s July 16 decision to approve the drug was based in part on the results of the three-year iPrEx trial, which showed that Truvada’s daily use by men who have sex with men reduced instances of HIV infection by 42 percent — 90 percent for participants who took the medication consistently enough to have detectable drug levels in their body.
The findings were based on the 2,499 HIV-negative men and transgender women who have sex with men in six countries enrolled in the study.
Pedro Goicochea, an investigator for the iPrEx study, says Truvada is currently available for use as a PrEP only in the United States, but he’s optimistic that it will be implemented in other parts of the world.
“This speeds up the process of issues and guidelines for other countries on the use of Truvada for PrEP,” he says. “At this very moment there is another study taking place in France where they are evaluating the intermittent use of Truvada. I’m sure that after they have results it will inform any decision that France makes. We also received comment from the College of Physicians in the UK where discussions are starting to take place.”
“Of course, PrEP is very controversial in parts of the world, even in the US,” Goicochea acknowledges. “It’ll take time to come to agreement, but I think this decision from the FDA will start to open the discussion.”
Goicochea says some critics have expressed concern that people taking the drug will have sex more often and freely and engage in unsafe sex leading to higher instances of other sexually transmitted infections. But, he says, condom use actually increased during the study. “But of course, this is under the conditions of the clinical trial with monthly visits. So participants were consulted and given condom supplies on a monthly basis,” he says. “They also received regular checkups and regular HIV testing.”
Dr Richard Lester, the medical head of STI/HIV services at the BC Centre for Disease Control (BCCD), says the evidence from the Truvada study is too good to ignore. But he can’t speculate when PrEP might be available in British Columbia.
“In the BCCD and the BC Centre for Excellence in HIV/AIDS there are a lot of comprehensive HIV-control strategies that are either being implemented or considered,” Lester says. “PrEP is certainly now an evidence-based strategy. Certainly the most relevant to our BC practices is the iPrEx studies of men who have sex with men taking the medication prophylactically to prevent infection when they are at risk.”
“I can’t say today when and where PrEP will fit in,” Lester says. “I think that there’s definitely a potential room for a move. Even though new infections are reducing year by year at the moment, they are still not as low as they could be, and there are people who are negative but want more control to protect themselves.”
Ultimately, the federal government would have to approve Truvada for use as a preventive medication, Lester says.
Bill Coleman, a Vancouver therapist who has worked with the HIV community for more than 25 years, is excited at the prospect of a new tool in HIV prevention.
“The biggest problem for almost 30 years has been one message — which is ‘use a condom’ — and that doesn’t work for everyone,” Coleman says. “If you look at all the different options talked about for gay men, one is using a condom, another might be I’ll fuck and not get fucked because that’s less risky, or I’ll have sex with poz guys with undetectable viral loads. There is nPEP as an option if a person ends up in a risky situation, and now there’s PrEP. So if you combine all those together, you can reduce the risk quite a bit.”
The Ministry of Health and the BC Centre for Excellence in HIV/AIDS recently launched an 18-month pilot project called Non-Occupational Post-Exposure Prophylaxis (nPEP). Under nPEP the BC government will now cover the costs for treatments following high-risk exposures to HIV that didn’t occur at work, such as unprotected sex and intravenous drug use.
“I think that [PrEP] provides an additional option for people to reduce the risk of getting HIV, and I think anything that lowers risks is good for everyone,” says Shawn Syms, an HIV/STI advocacy journalist.
“Things to bear in mind,” he notes, “are that, regardless of the sex that people have, it’s pretty much been demonstrated that the vast majority of people who don’t have HIV don’t want to get it, and the vast majority of people who have it don’t want to spread it.”
Syms hopes the new treatment will lessen the psychological and legal impact of HIV criminalization. It is still considered a crime in Canada for HIV-positive people to have unprotected sex without disclosing their status if there’s a significant risk of transmitting the virus.
“I hope that medical developments like this will reduce the incidents of HIV criminalization in time because they represent one more way that HIV advocates can demonstrate that the risk of HIV transmission is getting lower and lower,” Syms says. “Anything that makes HIV harder to transmit can improve the lot of HIV-positive people.”
According to Truvada’s medication guide, the most common side effects for people who take it as PrEP include abdominal pain, headaches and decreased weight. Serious side effects may include build-up of acid in the blood stream, severe liver problems, bone problems, changes in body fat, changes in the immune system, and worsening of an existing hepatitis B infection. These serious side effects, however, were uncommon in the clinical trials.
Truvada’s manufacturer, Gilead Sciences, also warns that if individuals unknowingly acquire HIV while taking the medication as a PrEP, they may develop resistance to Truvada, making the HIV harder to treat.
 Why you can trust Xtra
Why you can trust Xtra


