Chlamydia is now the number one reported sexually transmitted infection (STI) in Ottawa, after three years of steadily increasing rates.
In response to this rise in reported cases, Ottawa Public Health (OPH) has reintroduced a confidential bathhouse testing project in an attempt to curb the spread of the sometimes-silent bacterial infection in the gay community.
Men who frequent Steamworks or Club Ottawa can fill out a simple survey, then provide contact info and a urine sample for an STI test.
The University of Ottawa’s Dr Patrick O’Byrne, who conceptualized the self-directed bathhouse testing project in 2007 with Rick Dias of OPH’s Sexual Health Centres, says that if someone does not want to see a clinician, the bathhouse is an option.
The number of cases of chlamydia has risen steadily in Ontario, the UK, the US and Australia over the past 10 years. In 2012, chlamydia accounted for 82.1 percent of all reported STIs in Ottawa and 63 percent in Toronto.
OPH reports that between 2005 and 2009, it recorded 1,618 cases of chlamydia on average per year. That number jumped to 2,314 cases in 2010.
Dr Vera Etches, the City of Ottawa’s associate medical officer of health, says it is impossible to know the exact number of chlamydia cases in Ottawa’s gay men as the sexual orientation of someone tested at a sexual health clinic is not recorded unless they test positive for HIV.
“Our data comes from a laboratory requisition form,” she explains. “If you’ve gone to the doctor or the sexual health clinic, we don’t write, ‘This is a gay man and this is not.’”
Though the transmission rate in the gay community may be hard to pinpoint, O’Byrne felt there was enough cause for concern to reintroduce bathhouse testing.
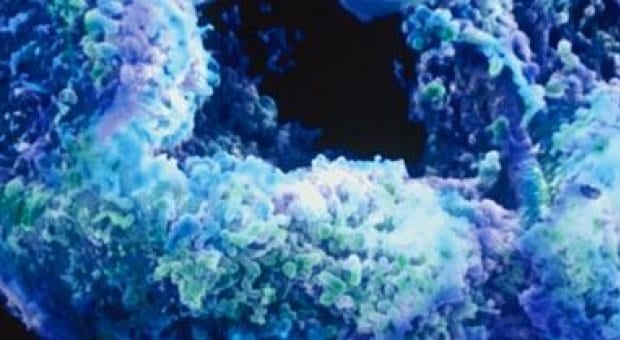
Chlamydia is a bacterial infection transmitted through giving or receiving oral, anal and vaginal sex.
Symptoms for men include a burning sensation when urinating, testicular pain, penile discharge, anal discomfort and a persistent sore throat. In women, symptoms of chlamydia include pelvic and abdominal pain.
Andrew Brett, communications director for the AIDS Committee of Toronto (ACT), says that although chlamydia is predominantly transmitted among heterosexuals, the rise of chlamydia concerns ACT because any STI makes a person more vulnerable to HIV infection and vice-versa.
“Sometimes people talk about other methods to avoid HIV; for example, having oral sex because it carries a lower risk of HIV transmission,” Brett explains. “That is one of the other ways you can contract another STI. That’s why it is important not to only think about HIV but other STIs as well.”
Etches says that the rise in reported cases doesn’t necessarily mean there are more people infected with chlamydia. An increase in the number of people undergoing tests also corresponds with the spike in recorded chlamydia cases, she says. Simple urine tests have replaced the old method of swabbing the vagina or penis to test for infection, encouraging more people to be tested and resulting in more reported cases.
The OPH’s Get Tested, Why Not? self-reporting website allows Ottawans to take a risk-assessment quiz and print a lab requisition form. Concerned individuals can take the form to any lab listed on the site and submit a urine sample, eliminating the need to see a family doctor or make an appointment, Etches says.
Dr Mark Gilbert, a physician and epidemiologist with British Columbia’s Centre for Disease Control, says cases of chlamydia in BC have held steady for years, with the prevalence rate among men who have sex with men consistently at five to seven percent each year, which he still considers high.
Gilbert says it is encouraging that more people are undergoing tests and therefore avoiding complications from chlamydia, such as ectopic pregnancy in women.
While Gilbert applauds testing, he says a urine test will not detect an anal chlamydia infection.
“We know that chlamydia can often be carried in the anus or rectum. It’s important that people are getting regular tests,” he says.
Etches points out that using a condom reduces the risk of transmitting most STIs, including chlamydia.
Ottawa Public Health report, 2011 by XO_reporter

 Why you can trust Xtra
Why you can trust Xtra


